Different Approaches to Managing Pain


Biomedical vs. biopsychosocial model of pain management
There is a paradigm shift happening in the model of care for chronic pain. The widespread model that is still in use today is the biomedical model of care. It looks at medication of various strengths (e.g., non-opioid to opioids) to control pain, and uses rehabilitation (e.g., psychotherapy, physiotherapy) +/- injections (or vice versa) and surgery as viable options to use in conjunction with or following medication management. With the biomedical model including pharmaceuticals and invasive procedures, stress and anxiety continually climb!
The issue with the biomedical model of care is that there is a large emphasis on the biological aspect of why pain occurs, when we now know that there are many other influencing factors to pain! Pain cannot be managed without movement, pleasure, or purpose. Lifestyle can largely impact pain, such as sleep patterns, diet choices, smoking, drinking, and recreational drug use. One of the leading causes of chronic pain is stress.
To address pain on a more comprehensive scale, there is a shift in healthcare toward adopting the biopsychosocial model of care for chronic pain. In this model, pain is presented as a journey, with the goal being the ability to manage pain independently. It uses softer terms such as “persistent” instead of “chronic” to help decrease stress or anxiety. It takes into account all factors that affect one’s pain experience:
BIO = physical (tissue level, medication management, rehabilitation)
PSYCHO = mental (thoughts, emotions)
SOCIAL = support in life, sense of purpose/belonging (family/friends & role within social circles, social network & diversity/size of them, interaction with society, how often go into community)
The more research that is conducted on chronic, or persistent, pain, the more complex we see this issue being. Our model of care needs to be much more holistic, and not focus on the bio piece.
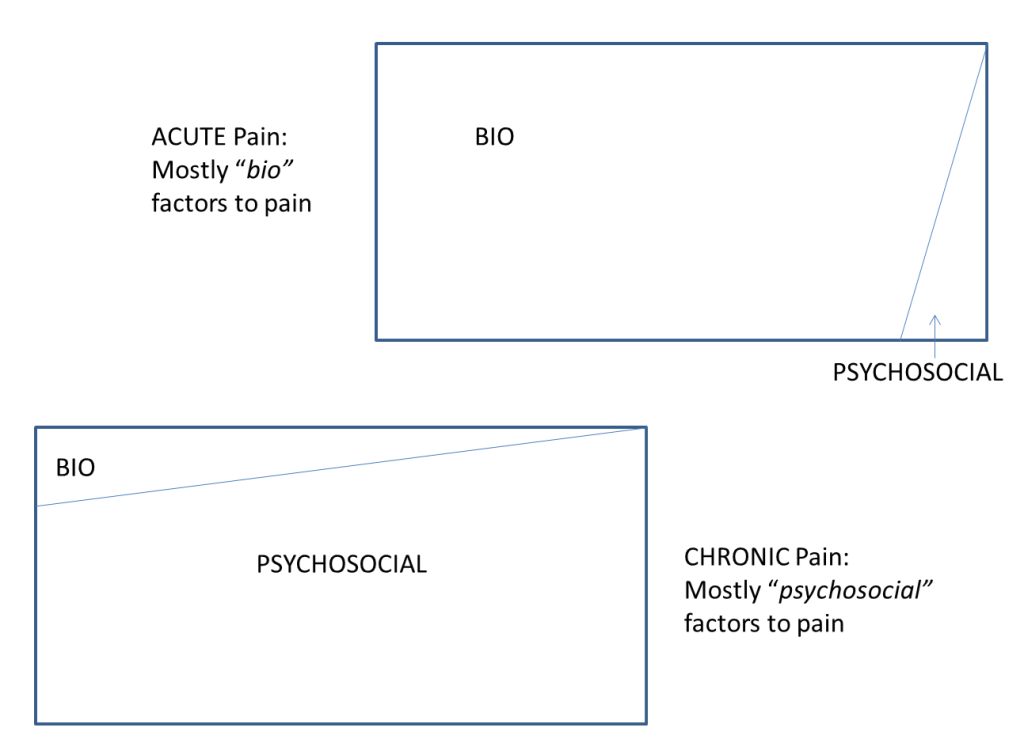
This website will focus heavily on the psychosocial piece, as the bio piece is most known and applied in healthcare today. Truthfully, in persistent pain there is very little of the bio piece that is even relevant, as all tissues heal over time! If you are curious about furthering your knowledge about medication, your pharmacist would be an excellent point of contact. For questions about injections or surgery, you may wish to speak to your doctor or nurse. Truthfully, most people with chronic pain have already explored these avenues, probably much more than necessary. When you hear multiple diagnoses, multiple treatments that are needed, and medication keeps increasing, those are all part of your experiences that make your nervous system more sensitive to pain!